How much does a Family Physician work?
I finished my first year as an attending! I work in an academic and urban setting and do a unique version of full-spectrum family medicine: I see patients of all ages in a clinic, I take care of adults in the inpatient setting as a hospitalist, and I deliver pregnant women as a laborist in addition to post-partum rounding on newborns in the hospital (I am not obliged but often come in to see my personal patients in these hospital settings as well); I work days and nights; moreover, part of my job is to teach medical students and resident family physicians.
Many residents comment, “Henry, you work a lot!” I love what I am doing and simply can’t imagine doing anything else; but the question remains, “Do I work more than the average family doctor?”
How many hours do I work?
In order to calculate how many hours I spend working, I needed to estimate how my work days are spent. Some days I do clinic, some days I do OB (obstetrics) and MCH (maternal child health), other days I do FMIS (family medicine inpatient service), and some days I do all three! A quick run-down:
- Typical clinic day [9.5-10.5h day]
- 7:30am – arrive in clinic, work on emails, sign or fill out faxed forms, finish charts, EMR tasks (“paper work”)
- 8:30am – begin morning clinic
- 12 to 12:30pm – finish clinic, get lunch, watch a lecture, attend a meeting, and/or resume “paper work”
- 1:30pm – begin afternoon clinic
- 4:30 – 5pm – finish clinic, resume “paper work”
- 6pm – head home
- Typical MCH (obstetrics + postpartum/newborn care) day (least regularly structured, below is a rough estimate) [10-11h day]
- 7:30am – arrive in the hospital, receive signout from night attending
- 8am – start post-partum rounding on new moms and newborns with residents; circumcisions
- 10am – see triage patients and laboring patients
- 6pm – signout to night attending
- Typical FMIS day (also a rough estimate) [12h shift]
- 7am – arrive in hospital, receive signout from night attending
- 8am – start bedside rounding with resident Team 1
- 11am – table round with resident Team 2; then see the patients on Team 2 by myself
- 1pm – see new admits, precept admissions, coordinating discharges
- 7pm – signout to night attending
Sometimes I work these settings for a whole day or part of a day. I also do a considerable amount of nights. To make my calculations easier, I portioned these settings into “shifts”: morning, afternoon, and night. I then calculated hours spent per shift. With data I recorded over 6 months, I created a spreadsheet (that anyone could view if you are really piqued): link here.
Assumptions and notes for my calculation:
- “Paper work” – is very difficult to calculate:
- It involves literal paper work: signing or reading things faxed to the clinic, signing orders, filling out forms (disability, home health, government/state forms, etc), physical therapy orders, and anything that requires a doctor’s input for a patient.
- The electronic medical record (EMR) work includes: signing prescription refills, reading consultant notes and messages; reading lab and imaging results, and communicating with patients about these results, etc.
- Then there’s time needed to finish the clinic visit chart notes themselves.
- Moreover, since I am in an academic setting, there are resident clinic notes to be read and cosigned, resident labs and imaging to supervise, and communication with residents about patient care or evaluations.
- There needs to be time to schedule and set up shifts, meetings with other doctors, committees, etc.
- Lastly, emails take significant time: patient care, academic topics, etc.
- Every clinic session is 3.5 hours of patient encounter time, but I add 1.5 hours per shift to include associated charting and “paper work.” I come in 1 hour early to do this and spend about an 1 hour after clinic as well. This number incorporates lunch time as well because I am usually working through lunch. In contrast, some physicians go home right after clinic– they choose to do charting and “paper work” after their children go to sleep, around 8-11pm (so I hear… We don’t have kids yet).
- Precepting residents takes time, but overall less “paper work,” so I calculate the hours per session as less.
- Admin is pure time (plus half of lunch) + 0.5h for the time I get there earlier or spend afterwards to work on stuff.
- MCH and FMIS really don’t include anytime outside the hospital because I don’t really chart or do patient tasks outside the shift time. I usually finish all charting/paper work while in the hospital before I leave.
- Extra hours is a category the most inaccurate. It includes formal hours of teaching of residents and med students, EKG teaching, meetings, workshops, scheduling meetings, academic meetings, CME lectures, etc. I try not to double-account this time with “paper-work” or admin time.
Statistics
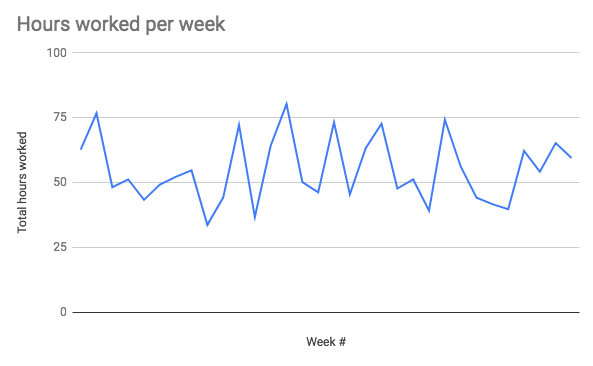
- Hours worked:
- I averaged 54.9 hours of work per week
- I worked a range of 33-80 hours per week
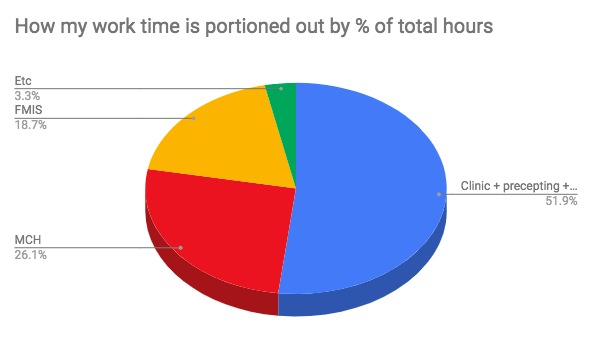
- % of total working time breakdown:
- I work 51.9% of my time in clinic (which includes seeing patients, admin time, precepting and “paper work”)
- I work 26% of my time on MCH (labor and delivery, post-partum rounding)
- I work 18.7% of my time on FMIS (adult inpatient medicine)
- Breakdown from a week perspective (the average over 32 weeks):
- 3.5 clinic sessions per week
- 1.5 precepting sessions per week
- 1 admin session per week (0.92)
- 1 Saturday 24-h OB shift every 10.7 weeks
- 1 OB overnight every 2.3 weeks
- ~3-day or night stretch of FMIS every 4 weeks
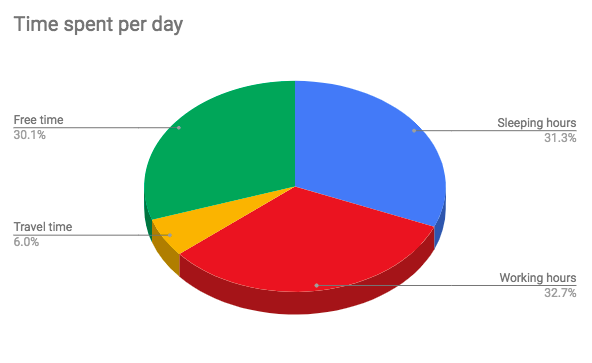
- Overnights:
- I work on average 2 overnights every 3 weeks
- I work on average 3 twenty-four-hour shifts every 5 weeks
- 18.33% of my total working time is working overnight
- 52% of my OB time is overnight
- 26% of my FMIS time is overnight
Discussion
I did a quick literature review of studies about physician work hours. The hours worked “average” ranged from 52 to 60 hours per week. A 2011 study in JAMA, using 2004-2005 data of physicians working, set the family physician hours worked in a year as the “average” in which other specialties are compared to: family doctors work 2,524 hours per year total. Comparisons for example: vascular surgeons work 888 more hours; while dermatologists work 346 less hours, relative to family doctors. (If I extrapolated my data and assume I work 48 weeks per year, I would work 2,635 hours per year; which is 111 more hours than the 2011 JAMA article family doctor average).
I think that overall my personal data is likely underestimating how much I work– I was fairly conservative with my estimations. However, it is within a reasonable range compared to the estimates in the studies I read. If I have more time, I would like to see a breakdown of how much doctors work overnight. As not a designated nocturnist, I am guessing I work more nights than most family doctors (18.3% of my total working time is overnight; 52% of my OB time is overnight).
In conclusion, I work marginally more than the average family doctor, but well within the range of average. I can make a similar statement if I compare my hours to other specialties as a whole (all doctors vs. just family doctors). I likely am working nights above the average for family doctors.
Burnout & Well-being
The next step would be comparing my quality of life to others in relation to hours worked. Burnout, well-being, and resilience are topics in full vogue right now (and rightly so). Interestingly, an article summarized a study from The Annals of Family Medicine, showing that the more full-spectrum a family physician works, the less burnout: “comprehensiveness is associated with less burnout, which is critical in the context of improving access to good quality, affordable care while maintaining physician wellness.” Here, I quote formally from that study: “practice characteristics significantly associated with lower odds of burnout were practicing inpatient medicine (OR = 0.70; 95% CI, 0.56–0.87; P = .0017) and obstetrics (OR = 0.64; 95% CI, 0.47–0.88; P = .0058).”
Clayton Christensen’s book, “How Will You Measure Your Life?” talks about satisfaction in the context of work. There are two types of factors contributing to this: hygiene factors and motivation factors. “Hygiene factors” if not done right, will causes us to be dissatisfied: poor status, compensation, job security, work conditions, company policies, supervisory practices make workers unhappy. However, even if hygiene factors are improved, you won’t automatically love your job; you just won’t hate it anymore. Christensen recalls Frederick Herzberg’s research and names “motivators” as another factor for job satisfaction. Motivation factors include: challenging work, recognition, responsibility, personal growth– very inward qualities. Problems arise when you prioritize hygiene factors over personal motivators (ie. “I’ll work a high-paying job and then when I pay off my loans, will work to save the world!”). Deferring real passions can lead to burnout.
I don’t have the data, but qualitatively I am pretty sure I am pretty happy so far. :D Paper work is a drag, but I seldom feel like I am not doing what I am called to do in this life. My favorite weeks (and even days) are when I get to see patients in all different settings and teach residents at the same time. A particularly memorable day, mixed the joy of delivering two babies in the morning, with the privilege of being with the family of a personal patient of mine passing away in the ICU, and the excitement of precepting residents in clinic in the afternoon (including doing some procedures); all ending with a quick lecture. It was hard, but I can’t imagine doing anything else!
- Burnout and Scope article – Weidner AKH, Phillips RL, Fang B, Peterson LE. Burnout and Scope of Practice in New Family Physicians. Ann Fam Med. 2018;16(3):200-205.
- “How Will You Measure Your Life?” – by Clayton M. Christensen
- “What do you love about being a family physician?” – “I become part of their lives and they become part of mine.”
- “What is a typical day like for you as a family physician?” – a really interesting article looking qualitatively what different family doctors do on a typical day
- Why Doctors Hate Their Computers – by Atul Guwande in an article from The New Yorker
- Tethered to the EHR: Primary Care Physician Workload Assessment Using EHR Event Log Data and Time-Motion Observations – ambulatory clinic doctors worked on average 11.9 hours per day, 1.4 hours are spent outside the clinic on the EHR
- Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties – this paper states doctors spend 1-2 hours of after-hours work each night
- Researchers Explore Diminishing Scope of FP Practice – “Once kids, OB, procedures, urgent care and inpatient care are removed, many family physicians have become outpatient-only managers of adult chronic disease.”
- Reclaiming Family Medicine’s Broad Scope Benefits Everyone – physician specialties have expanded from 15 to 130 types of doctors over time
- My quick literature review – on hours doctors work per week

Leave a Reply